Parent & Caregiver Open House
December 17 | 6:00–7:00 PM
Tour the facility, meet our department leaders, and get all your questions answered.
RSVP NowTransitioning ABA or therapies? Fast-Track Intake available. Talk to Intake Today
Personalized care for children and families living with autism and other developmental conditions.
Stay connected with what's happening at The Talcott Center — from community events to the latest news and updates.
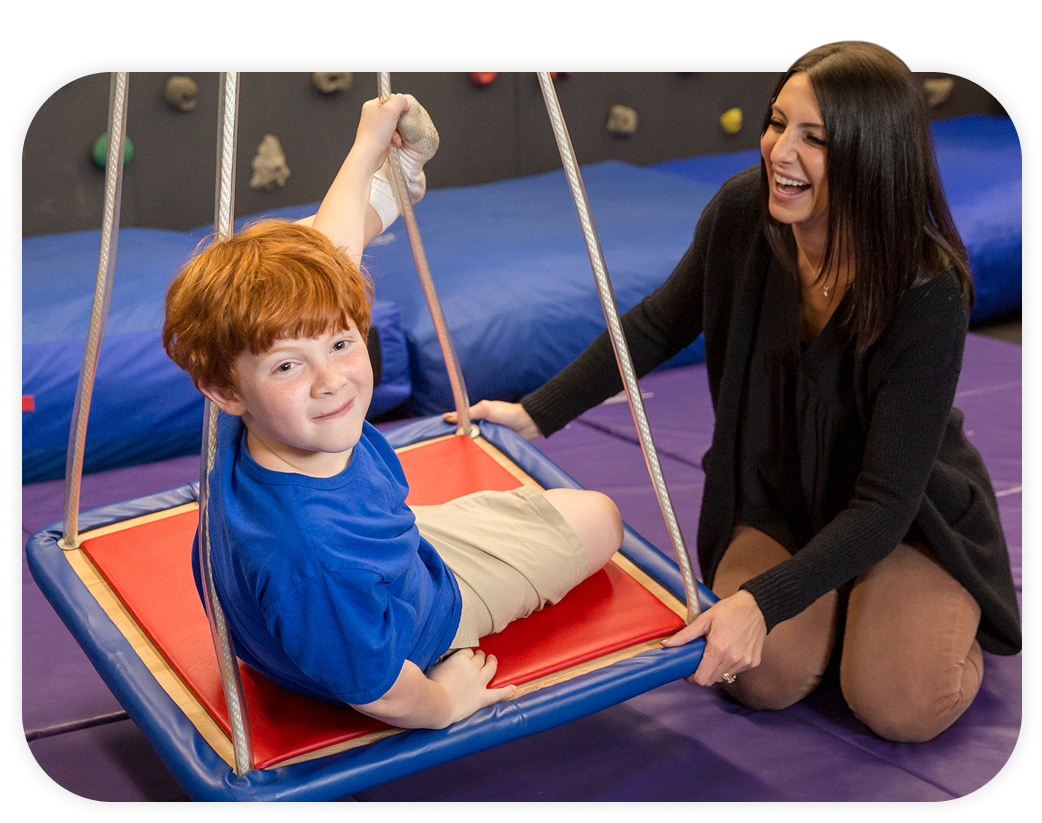
Through comprehensive therapy services and family-focused programming, we help your child develop essential life skills while keeping you central to the plan of care.
Evidence-based protocols for measurable skill development.
Experts who truly understand, embrace, and affirm neurodiversity.
Coordinated support to simplify therapy and strengthen family bonds.

Our interdisciplinary team approach means your child benefits from coordinated support across ABA, OT, SLP, and PT — all working together under one roof.
Learn More TodayThese testimonials reflect the care, trust, and life-changing progress that Talcott families experience every day.
Your child’s journey at The Talcott Center starts with a thorough and collaborative assessment process coordinated by our interdisciplinary clinical team.
Depending on your child’s specific needs, this may involve occupational, speech, physical therapists, and/or behavior analysts.
Together, we’ll map out a clear, individualized plan of care to ensure effective treatment outcomes for your child.
Our proven therapy services include:
Teaches essential skills through proven, compassionate methods – improving daily routines and behaviors.
Enhances language, social communication, and cognitive development for better
interactions at home and school.
Boosts everyday skills, from self-care and play to succeeding at school.
Develops strength, coordination, and motor planning, making daily activities easier and more enjoyable.
Helps overcome feeding difficulties with gentle, supportive approaches.
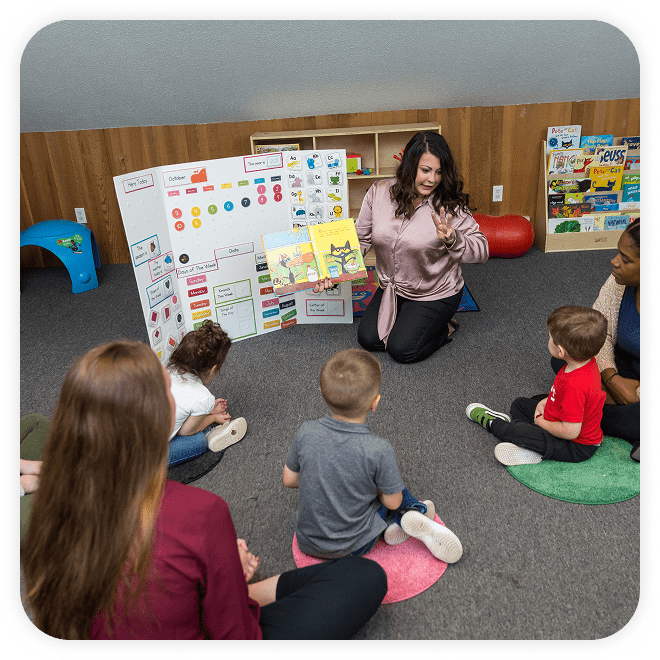
Full-day, intensive support designed specifically for children aged 2–6, integrating multiple therapies seamlessly.
Our Comprehensive Autism Day Program blends intensive 1:1 ABA therapy with occupational, speech, and physical therapies in a nurturing environment – ensuring holistic growth and school readiness.
Learn More Today
Your child deserves a place where they feel truly seen and valued. Our group programs offer exactly that — a supportive, joyful peer setting in which each child’s individuality is celebrated.
With small group sizes, your child receives focused attention to grow their confidence and social skills.
Intensive programs offered during school vacations and holidays to maintain your child’s progress.
Learn More Today
Our fun, immersive therapeutic summer program where your child will build social, sensory, and emotional skills while making summer memories that last.
Learn More Today



Since 2004, families like yours have trusted The Talcott Center because we genuinely understand — and continually respond to — the evolving needs of children and their parents.
Every expansion of our services, investment in new therapies, or upgrade to our facilities has one purpose: ensuring your child’s ongoing success and your family’s peace of mind.
Our mission is simple and heartfelt — to enhance and empower your child’s life by fostering independence, strengthening knowledge and building confidence.
Take the first step. Fill out this form to connect with our team and learn how Talcott can support your family’s journey.
Located conveniently in Farmington, CT, our inviting, state-of-the-art facility offers over 15,000 square feet thoughtfully designed to feel warm, calm, and supportive.
From the serene natural surroundings outside to the welcoming atmosphere within, your family will immediately feel at ease — making each visit comfortable and positive.
